Antimicrobial resistance (AMR)
We rely on a type of medicine known as antimicrobials to treat many common diseases, including TB (tuberculosis) and chest infections. The overuse and misuse of these treatments is making them less effective. This is known as antimicrobial resistance. It is one of the biggest challenges the world currently faces.
Content Table
What are antimicrobials?
Antimicrobials – including antibiotics, antivirals, antifungals and antiparasitics, are used to fight the bugs (pathogens) that cause many common diseases. They are also commonly used during surgery to prevent infections and during cancer chemotherapy.
What is antimicrobial resistance?
Using this kind of medication incorrectly and overusing it is causing the bugs it targets to become resistant to the medicine that has previously successfully treated them.
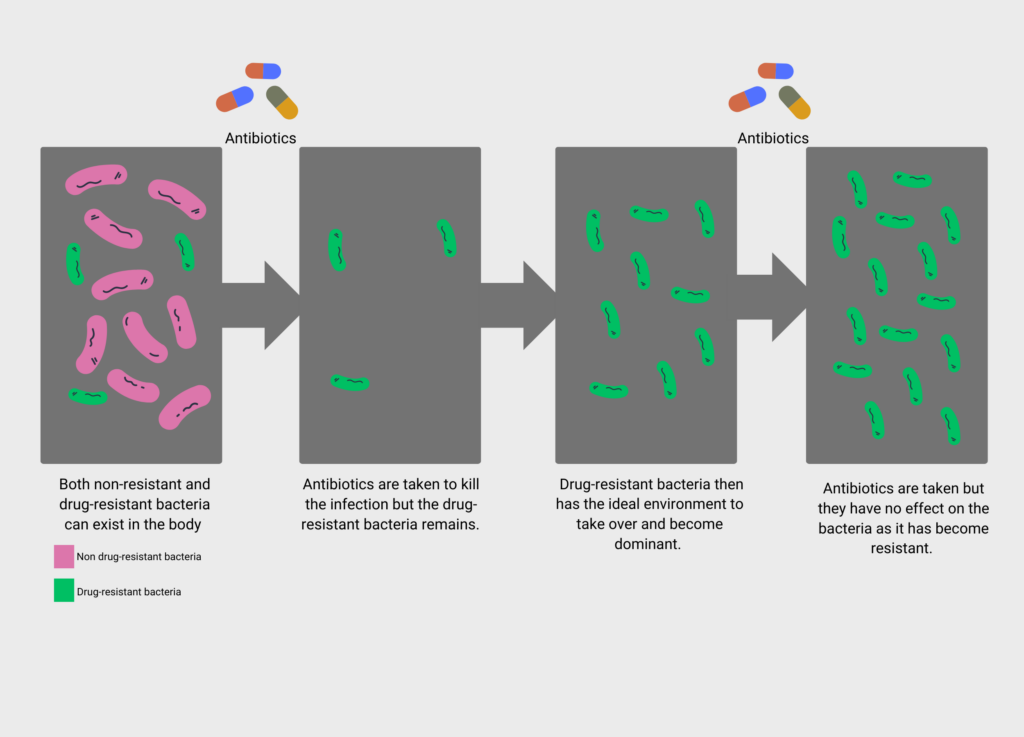
This happens over time when the bacteria, fungi, viruses, and parasites that cause illness change to avoid being killed by antimicrobials. These resistant strains then multiply and the resistance spreads.
How does drug-resistant bacteria become dominant?
Why is this happening?
Drug resistance does happen naturally – bacteria are designed to avoid death and will keep evolving to do so. However, from a healthcare perspective, this process is being sped up. This is due to the antimicrobials being:
- Overused: . They are used extensively to treat pets and livestock, such as cattle. Antifungals have been widely used as a pesticide to manage fungal diseases affecting several crops. Resistant bacteria have been found in lakes, rivers and oceans. Experts believe this has come from discharge flowing from hospitals, farms, or sewage systems. People are therefore becoming more exposed to resistant bacteria. As the use of antimicrobials grows, the presence of antimicrobial-resistant bacteria also grows.
- Misused: For example, when someone stops the prescribed course of the drug too soon or when they are given for illnesses caused by things they cannot treat, such as giving antibiotics for viral infections like colds and flu.
Drug availability and development is also contributing to the problem:
- There is a shortage of replacement antibiotics that can be used when strains of bacteria become resistant.
- There are even fewer which target super resistant strains of bacteria.
- There are not many alternative products being developed.
Why is it important?
Without effective antimicrobials, the success of modern medicine is at risk. The World Health Organization (WHO) has identified this as one of the top 10 global public health threats facing humanity.
If resistance continues to increase, infections could become more severe and last for longer as they will become difficult to treat. This could lead to longer hospital stays and higher death rates.
Without action, we will be unable to treat infections and routine operations could become deadly. This will affect all of us.
What areas of health are affected by this?
Antimicrobials are used to treat many conditions. For lung diseases, this includes TB, pneumonia, bronchiectasis and cystic fibrosis. Other conditions include HIV/AIDS, malaria, sexually transmitted infections, urinary tract infections, chest infections, bloodstream infections, food poisoning and fungal infections, such as aspergillosis.
Routine surgery— such as caesarean sections, hip and knee replacements, heart surgery — and cancer treatments, such as chemotherapy, also rely on antibiotics to prevent infections before, during and after procedures.
If you have a lung condition that often causes chest infections, you may need antibiotics to help manage your symptoms. You may be concerned that taking antibiotics can make bacteria become more resistant. Bacteria will not always become resistant, and so it is possible in many cases to use the same antibiotic successfully for many years. If the bacteria in your sputum are resistant to an antibiotic, your doctor will advise you if you need to take a different antibiotic.
It is important to only use antibiotics when they are really needed, such as when you have an exacerbation or your symptoms are severe. Ask your clinician if you are not sure how to identify this. It is important to work with your clinician on a clear symptom management plan including the type and length of antibiotic duration and to follow this carefully when required. Avoid using antibiotics if you do not have an infection or if your symptoms are under good control.
What can be done to prevent it?
Many countries are adopting national plans to tackle growing antimicrobial resistance. Strategies include:
- preventing infections and measuring infection control,
- improving early diagnosis,
- encouraging the appropriate use of antimicrobials and only prescribing when there is an infection they are able to treat,
- working across all sectors to achieve the best health outcomes for people, animals, plants, and their shared environment,
- encouraging the development of alternatives to current antimicrobials.
There is a need for a coordinated action across the world. The World Health Organization (WHO) is calling for greater funding for research and development into new antimicrobial medicines, vaccines and diagnostic tools.
In 2015, countries across the world signed up to the Global Action Plan on AMR and committed to developing national action plans.
Further information
Visit the WHO website for more information on the WHO Global Action Plan on AMR and other coordinated strategies that are happening across the world.




