Nebuliser and inhaler guide
This guide is designed to help adults understand how to use nebulisers and inhalers, and how to choose a device that works best for you.
Content Table
What is inhaled medicine?
If you have lung conditions like bronchiectasis, asthma, or COPD, your doctor may prescribe medicine that you breathe in rather than swallowing or injecting. This way, the medicine goes straight to your lungs where it is needed.
Advantages of inhaled medicine include:
- The medicine is delivered directly to the airways, which means it can potentially act faster to improve symptoms.
- There is less medicine in the blood, compared to swallowing or injecting medicine, which can help to reduce any potential side-effects.
What is a nebuliser?
A nebuliser turns liquid medicine into a fine mist that you can breathe in through a mask or mouthpiece. You add medicine to the device each time you use it.
What is an inhaler?
An inhaler is a small, hand-held device that delivers medicine as a spray or powder. Types of inhalers include:
- Pressurised metered dose inhalers (pMDIs)
- Dry powder inhalers (DPIs)
- Soft mist inhalers (SMIs)
Questions a healthcare professional might ask when deciding on the best inhaler
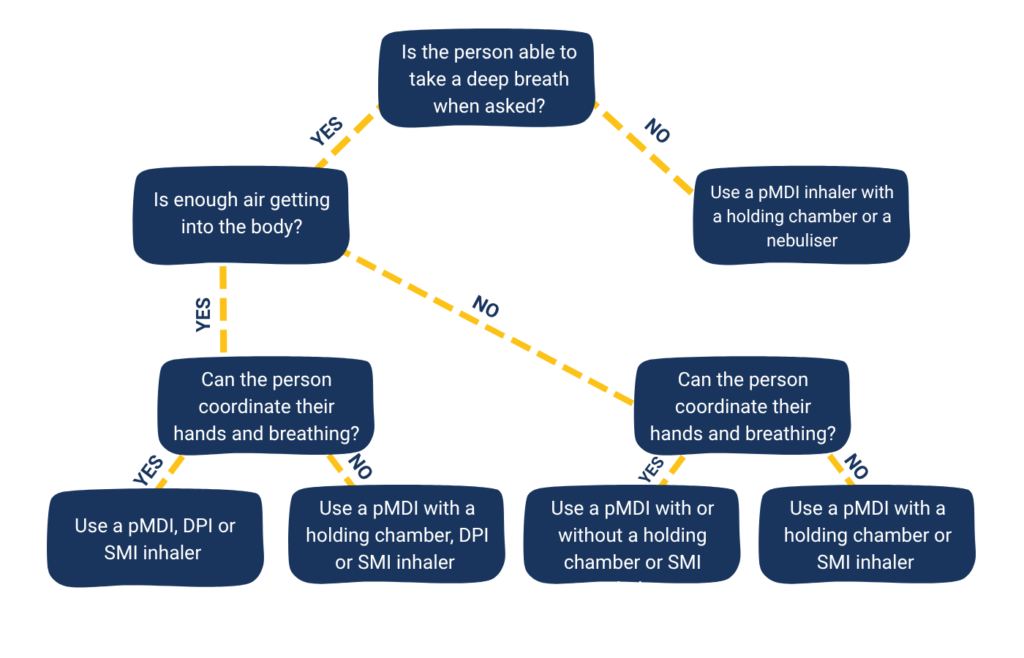
When is it better to use a nebuliser?
- A nebuliser is better when the medicine includes a large amount of liquid (such as antibiotics for infections or salt solutions for thick mucus).
- It is also better for people who have trouble using inhalers.
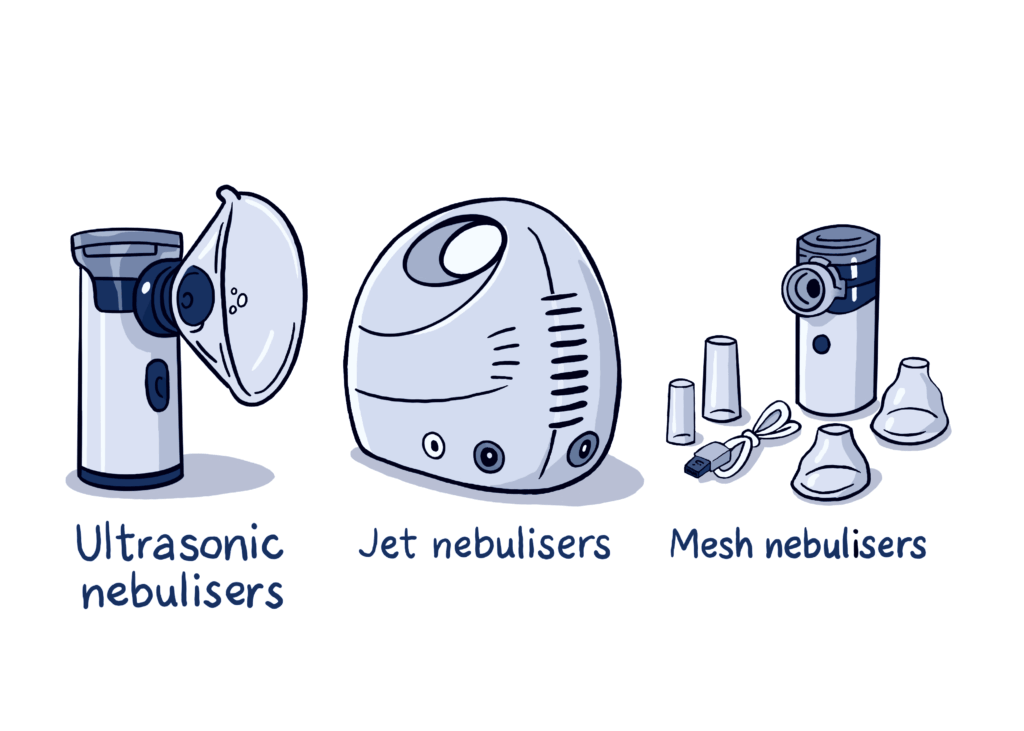
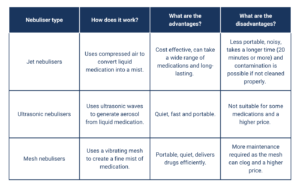
Nebuliser types
Nebuliser types work differently and suit different needs:
Ultrasonic nebuliser
- Consists of a power unit, with or without an electric fan.
- Ultrasonic with a fan: The fan helps deliver the mist more effectively
- Ultrasonic without a fan: The mist is pulled out of the nebuliser when you breathe in and out.
- The power unit converts electrical energy into sound waves, which makes a mist.
- Quieter medicine delivery and shorter treatment time than the jet nebulisers.
- Poor battery life, can overheat (which may damage antibiotics), effective only for solution medicines (does not work well for suspensions such as budesonide), the drug delivery depends on the angle the device is being held in.
Jet nebuliser
- Turns the medicine into a fine mist – in combination with an air compressor or a pressurised gas supply, which are commonly used in hospitals.
- Medicine is placed in a cup and a mouthpiece or face mask is used to breathe in the mist.
- They are less portable and can be noisy.
There are three main types of nebuliser technologies used for JET nebulisers that affect how well the medicine is delivered:
- Constant-output nebulisers
- Produce mist continuously, even when you are breathing out.
- This leads to high medicine waste and can mean the amount of medicine you receive varies.
- Breath-enhanced nebulisers
- Add extra air with the medicine when you breathe in, which improves delivery to the lungs.
- When you breathe out, a valve closes the vent, reducing medicine loss into the air.
- Breath-actuated nebulisers
- Only release medicine when you breathe in, giving you more of the medicine directly into the lungs.
- Some advanced models can track your breathing and adjust the way the medicine is delivered automatically.
- These may take longer but are very efficient at delivering the medicine to the lungs.
Mesh nebuliser
- Aerosol device that uses a mesh – a filter with tiny holes – to produce a very fine mist, making it more efficient at delivering the medicine in the body.
- Able to deliver precise doses of medicine with minimal waste.
- Battery operated and more lightweight than other devices.
- Portable and quicker at delivering the medicine compared to jet nebulisers.
- The mesh can get clogged, particularly by concentrated salt solutions or some antibiotics.
Choosing the right nebuliser
Choosing the right nebuliser can make a big difference in how well your treatment works. Good nebulisers meet international safety standards (like the International Organization for Standardization (ISO)) to make sure they work well and are safe to use. Here are some simple things to keep in mind:
- How easy it is to use and clean
- How fast it delivers the medicine
- How well you can use the device
- How easy it is to move around and how noisy it is
- Durability and cost
- The medicine you need – some only work in certain devices
- Whether the device can be disinfected.
Tip: You may need more than one device — one for home, another for travel.
Remember that as medicines change, the nebuliser type may need to change as well. It is important to keep on top of cleaning your nebuliser as clogged filters or meshes can affect how well the medicine is delivered.
For more tips, check the appendix and reference list at the end of this document.
Getting the most from your nebuliser treatment
To get the most effective treatment from a nebuliser, it is important that enough of the medicine reaches the lungs. One way to measure this is with something called the RDDR (Respirable Drug Delivery Rate), which shows how much of the drug could actually be delivered.
Choose a nebuliser with a high RDDR. As this number is not often shared by manufacturers, you can also look for a nebuliser that produces very small mist droplets (1 to 5 micrometers) and has a high mist output (0.2 to 0.5 mL per minute). These features help ensure more of the medicine gets into the lungs where it is needed.
You can also ask your clinician, particularly those who specialise in your condition, about which nebulisers meet the criteria for being efficient.
Face mask vs mouthpiece
- Mouthpieces waste less medicine and help to direct it straight to the lungs.
- A face mask should be avoided when using steroid or medicines that calm down overactive muscles and glands in the airways (known as anticholinergic medicines) to avoid affecting the skin or eyes.
How to use a nebuliser (step-by-step)
Before you start:
- Wash your hands.
- Set up the nebuliser (connect the tubing, mouthpiece or mask, medicine cup).
- Add the medicine as directed by your doctor.
During treatment:
- Sit upright to help the medicine reach your lungs.
- Place the mouthpiece in your mouth and close your lips around it, or secure the mask over your nose and mouth.
- Start the machine and breathe in slowly through your mouth, holding each breath for a few seconds before breathing out.
- Stay relaxed – you can watch TV or read a book to pass the time.
- Tap the nebuliser cup occasionally to ensure all the medicine is used.
After treatment:
- Turn off and clean all parts according to the manufacturer’s instructions. This usually involves washing with warm, soapy water and allowing the parts to air dry.
- Store the nebuliser parts in a clean, dry place until the next use.
Maintenance:
- Regular cleaning and disinfection according to manufacturer’s instructions
- Replace any worn or damaged parts as recommended by the manufacturer.
Safety tips:
- Only use medicines prescribed by your healthcare provider in your nebuliser.
- A nebuliser is intended for one patient only. However, a single compressor may be used for more than one person, providing each uses their own nebuliser handset.
- Follow the specific instructions provided by your healthcare provider and the nebuliser manufacturer.
- If you have any specific questions or concerns, it is always best to consult with your healthcare provider.
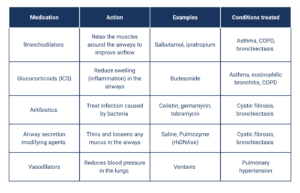
Mixing nebulised medicines
Some medicines can be mixed to save time. The table below specifies which medicines may be mixed together but always check with your doctor or pharmacist first.
This information was compiled with the help of EMBARC and members of the ELF bronchiectasis patient advisory group. EMBARC is a pan-European network committed to promoting clinical research and education in bronchiectasis, through sharing of protocols, research ideas and expertise.
With thanks to Dr. Noga Aharoni and Dr. Michal Shteinberg- Carmel medical center, Haifa, Israel and European Lung Foundation Bronchiectasis Patient Advisory Group members, Philip Alper and S Nadler for their contributions.
Thanks also to the following people for sharing information and expertise:
- Dr. Rosina Ledermüller, Global Senior Medical Advisor, Pari GmbH, Germany
- Beatriz Herrero-Cortina, Physiotherapy specialist, Hospital ValHebron, Barcelona, Spain
- Prof. Dr. Felix Ringshausen, Hannover Medical School and German Respiratory Society
Further scientific information can be found in these published articles:
- Elkins MR, Robinson M, Rose BR, et al.
A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis.
N Engl J Med. 2006; 354:229–240. - Wark P, McDonald VM.
Nebulised hypertonic saline for cystic fibrosis.
Cochrane Database Syst Rev. 2018; 9:CD001506. - Flume PA, O’Sullivan BP, Robinson KA, et al.
Cystic fibrosis pulmonary guidelines: chronic medicines for maintenance of lung health.
Am J Respir Crit Care Med. 2007; 176:957–969. - Herrero-Cortina B, Alcaraz V, Vilaró J, et al.
Impact of hypertonic saline solutions on sputum expectoration and their safety profile in patients with bronchiectasis: a randomized crossover trial.
J Aerosol Med Pulm Drug Deliv. 2018; 31:281–289. - Nicolson CH, Stirling RG, Borg BM, et al.
The long-term effect of inhaled hypertonic saline 6% in non-cystic fibrosis bronchiectasis.
Respir Med. 2012; 106:661–667. - Pasteur MC, Bilton D, Hill AT, et al.
British Thoracic Society guideline for non-CF bronchiectasis.
Thorax. 2010; 65(Suppl 1):i1–i58. - Laska IF, Crichton ML, Shoemark A, et al.
The efficacy and safety of inhaled antibiotics for the treatment of bronchiectasis in adults: a systematic review and meta-analysis.
Lancet Respir Med. 2019; 7(10):855–869. - Lavorini F, Fontana GA, Usmani OS.
New inhaler devices – the good, the bad and the ugly.
Respiration. 2014; 88(1):3–15. - Ringshausen FC, et al.
Management of adult bronchiectasis – Consensus-based Guidelines for the German Respiratory Society (DGP).
Pneumologie. 2024.