Allergic rhinitis or ‘hayfever’
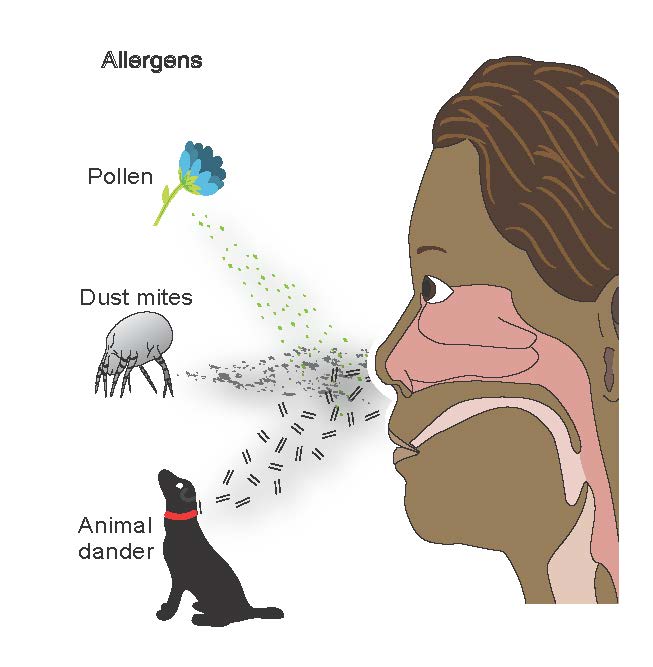
Allergic rhinitis is a disease in which the mucous membranes of the nose are swollen and irritated. This is caused by an allergy to grass or tree pollen, house dust mites or sometimes to mould. The lay term is “hay fever”, which is widely used but incorrect: allergic rhinitis has nothing to do with hay or with fever. Approximately 10–15% of 6–7-year-olds and 20–30% of teenagers and young adults have allergic rhinitis. Symptoms can vary from very mild to very serious.
What are the symptoms of allergic rhinitis?
Classical form:
- runny nose
- sneezing
- itchy nose and eyes
- red eyes in spring or summer
These symptoms are usually accompanied by allergy to tree (spring) or grass (summer) pollen, sometimes to weed pollens and fungal spores. This is particularly common in young adults.
Persistent form:
- persistent symptoms of stuffy (and sometimes runny) nose
- usually with cough and a general lack of energy
Allergic causes here include dust mites, pet dander and sometimes mould.
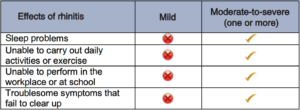
How are allergic rhinitis symptoms classified?
Symptoms are classed as “intermittent” if they occur for less than four days a week and last for fewer than four weeks. Symptoms that exist for longer than this are regarded as “persistent”.
What other problems can allergic rhinitis cause?
What is the relationship between allergic rhinitis and asthma?
Allergic rhinitis and asthma are very common allergic disorders and some clinicians think they are both part of a single “united airways” disease. Untreated allergic rhinitis increases the severity and symptoms of asthma. Patients with both asthma and allergic rhinitis have improved control of symptoms when both diseases are treated.
What are the external signs of allergic rhinitis?
The two main external signs are:
1. the “allergic shiners”, where the lower eyelids are darkened;
2. “allergic salute”, when an individual rubs their itchy nose.
When should you seek medical advice?
Allergic rhinitis can be treated effectively, so visit your doctor if your rhinitis is troubling you, particularly if you experience persistent or moderate-to-severe symptoms and you have associated features of asthma (cough, wheeze or tight chest).
How can allergic rhinitis be treated?
- Avoid irritants such as tobacco smoke.
- Allergen avoidance in the home is only possible with house dust mite or pet allergy. Avoidance of
house dust mites is only effective if a full package of allergen avoidance is being followed, including
mattress, pillow and duvet cover treatment, and a home visit by trained experts. Applying special bed
covers is not helpful on its own. Pet allergy can only be treated by removing the pet, which can be a
difficult decision. It may not be possible to avoid allergens when you visit other places. - Drug treatment:
- Mild or intermittent symptoms: antihistamine tablets or syrup (non-sedating antihistamines
are preferred because they do not cause drowsiness, e.g. loratadine or cetirizine). These
relieve rhinitis symptoms (particularly sneezing and runny nose) but are less effective for
blocked nose - Moderate-to-severe or persistent symptoms: nasal steroid spray (e.g. budesonide,
momethasone, fluticasone). Nasal steroids are more effective than antihistamines. They
have to be taken regularly to prevent symptoms. - Montelukast tablets may be used as additional medication in troublesome cases.
- Other drugs are ineffective (including cromoglycate).
- Mild or intermittent symptoms: antihistamine tablets or syrup (non-sedating antihistamines
- If such drug treatment is ineffective seek referral to an allergist, ear, nose and throat (ENT)
specialist or paediatrician. In severe cases, allergen-specific immunotherapy (“allergy shots”) can be
added. This is effective in most cases.