Alpha-1 antitrypsin deficiency
Alpha-1 antitrypsin (AAT) deficiency is a genetic condition which increases the risk of lung and/or liver diseases. People with AAT deficiency have low levels of AAT protein in their blood and are more likely to get lung disease earlier in their life than someone with higher levels of AAT. The most common lung disease that people with AAT deficiency are likely to get is chronic obstructive pulmonary disease (COPD). It is thought that less than 1 in 10 people with AAT deficiency have been diagnosed. This means that most people with the condition are unaware that they could benefit from changes to their lifestyle or medical help which could reduce their chances of getting lung disease.
Content Table
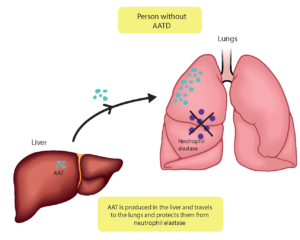
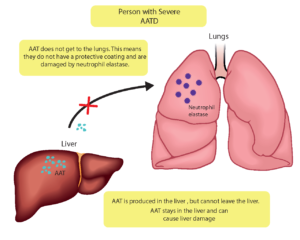
How does a lack of AAT cause lung disease?
AAT protein is made in the liver and released into the blood. It enters the lungs from the blood and its job is to protect the lung tissue from being damaged. It protects the lungs from another protein called neutrophil elastase, which is released by white blood cells. The job of neutrophil elastase is to destroy damaged cells and bacteria. AAT stops it from attacking healthy lung cells.
How can genes cause AAT deficiency?
DNA is a code that that makes up every part of our bodies. There are millions of tiny sections of this code and they each do different things. These small sections are called genes. We have two copies of almost all our DNA, one from each of our parents. AAT deficiency is caused when there is an error or abnormality in the code in one of the genes. This gene is called SERPINA1.
Severe AAT deficiency is called a ‘recessive’ condition. This is because there needs to be two abnormal copies of the gene to cause the condition. People who have one abnormal and one normal SERPINA1 gene are called carriers. They usually have an intermediate AAT deficiency this means their AAT levels are usually lower than normal, but not low enough to cause a serious risk of health problems. They can pass their one abnormal gene to their children, but they do not have the condition themselves.
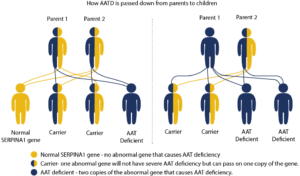
The children of two carriers can inherit two normal genes, one normal and one abnormal gene and become carriers themselves, or two abnormal genes and have AAT deficiency. This is shown in the diagram above. If a person with two abnormal genes has children, the children will either have the condition or be a carrier, depending on the SERPINA1 genes of the other parent as can be seen in the second diagram.
Several different abnormalities in the SERPINA1 gene have been found that result in different amounts of AAT protein being made. This means the condition can be more severe in some people than others.
Does having AAT deficiency mean that I have a disease?
Not really. AAT deficiency is a genetic condition which increases your risk for developing lung and/or liver diseases. Although, many people with AAT deficiency who do not smoke do not develop any disease and/or related symptoms.
How common is AAT deficiency?
Although AAT deficiency is thought of as a rare genetic condition, it is actually one of the most common inherited genetic conditions in some parts of the world, such as Europe.
In some Northern European countries, between 1 in 1,600 and 1 in 2,000 people are thought to have AAT deficiency; in some other regions, i.e. in South/East Europe, AAT deficiency is less frequent. Recent studies estimated that there are about 120,000 people in Europe with severe AAT deficiency.
The reason that people think it is rare is because the disease(s) associated with AAT deficiency are often not recognised or diagnosed. There is often a long delay before people are diagnosed with the condition even after visiting a doctor with symptoms. One scientific study found that a diagnosis of AAT deficiency was made on average 7 years after the first symptoms appeared.
The reasons that most people with lung disease associated with AAT deficiency are either not properly diagnosed or are never diagnosed include:
- Symptoms can be very different in different people;
- COPD, or asthma symptoms, can have many other causes;
- Liver diseases also can have many other causes
What are the symptoms of lung diseases associated with AAT deficiency?
AAT deficiency can cause similar lung symptoms to those seen in COPD or asthma.
Early symptoms include:
- Shortness of breath, either when doing something physical or when resting
- Cough; lots of mucus and saliva when you cough
- Liver diseases also can have many other causes
Many people with AAT deficiency have no symptoms, which makes it very difficult to diagnose. Therefore, guidelines suggest that all people with COPD or adult-onset asthma should be screened for AAT.
Symptoms in the liver or abnormalities caused by AAT deficiency either in infants, children or in adults may be jaundice and/or increased liver enzymes, or other symptoms like panniculitis (painful bumps under the skin), and inflammation of the fatty layer under the skin.
How will a doctor know that you have AAT deficiency?
A doctor who thinks someone might have AAT deficiency will take blood samples and do some laboratory tests that measure the amount of AAT in your blood. Gene testing can also be carried out to look at the SERPINA1 gene.
Because AAT deficiency is genetic and inherited, relatives of people with the condition are also likely to be carriers or to have the condition. Therefore, family members should also be told and tested. It may also be a good idea for partners to be tested, to find out whether there is a chance that any children will have AAT deficiency.
What are the next steps after AAT deficiency diagnosis?
After being diagnosed with AAT deficiency, your doctor should investigate whether AAT deficiency has affected your lungs, liver and general health and plan the best course of treatment.
The next step is to invite you to participate in the European Alpha-1 Antitrypsin International Registry (EARCO). European Commission have highlighted how important registries are for rare diseases. They are the only way to collect relevant information about the condition and its outcomes. EARCO is a platform for clinical research in AATD that will improve how the condition is managed in the near future. Please, ask your doctor about being included in EARCO (www.earco.org).
What can you do to prevent lung disease if you have AAT deficiency?
There are many things that people with AAT deficiency can do to ensure that they have a lower chance of getting lung disease or to slow its progress. Most of these involve trying to avoid damaging the lungs as there will not be enough AAT to protect them.
- Not smoking. Smoking is even more harmful to people with AAT deficiency,
as their lungs have less protection. - Avoiding highly polluted areas, for example by staying away from busy roads
at peak traffic times (for more information see the ELF factsheet ‘Outdoor air
pollution and the lungs’). - Avoiding exposure to fumes or inhaling toxic substances in the workplace
- Preventing bacterial and viral infections by avoiding people who are unwell
and by being careful about personal hygiene and having the prescribed
immunizations (e.g. flu vaccine). - Eating a balanced diet, rich in protein and vitamins
- Performing breathing exercises as recommended by your doctor.
How can AAT deficiency be treated?
AAT deficiency can be controlled but not cured. However, early diagnosis is very important so that treatment can begin as soon as possible.
General treatments for lung damage
Treatments that might be prescribed for patients with other respiratory problems such as asthma or COPD include the following:
Inhaled bronchodilators, either long-acting or short acting.
- Corticosteroids, preferably inhaled rather than taken orally
- Supplemental oxygen if needed.
- Pulmonary rehabilitation (below).
Pulmonary Rehabilitation
Pulmonary Rehabilitation (PR) is recommended for people with COPD as it improves exercise capacity, quality of life and breathlessness. Patients with COPD that is linked to AAT deficiency should be enrolled in PR programs both as inpatient and as out-patients, depending on local availability.
Treatment to replace AAT
Augmentation (replacement) therapy is available in many European countries. This involves a weekly dose of AAT that boosts the level of AAT in the blood and the lungs. Once the level is high enough, the AAT will start to protect the lungs. Patients must still stop smoking cigarettes and avoid environmental pollutants. Recent studies have demonstrated that replacement therapy slows the progression of emphysema, which is one of the components of COPD.
Surgical treatment for damaged lungs
Lung transplantation is an option for people with AAT deficiency who have serious lung disease. One or both lungs can be transplanted, and sometimes patients also receive a heart transplant. The number of lung transplants has increased a lot over the past 15 years.
Lung volume reduction (LVR) is where the diseased part of the lung is removed. It can be performed by surgery or more recently during bronchoscopy. This may help some AAT deficiency patients with lung disease, as it may reduce symptoms and improve exercise tolerance. Although LVR is not an alternative to lung transplantation, it can help patients to cope until a lung transplant is available.
Useful reference and websites
ERS Statement: diagnosis and treatment of pulmonary disease ina1-antitrypsin deficiency.
This document spells out the way in which doctors should recognise and treat AAT deficiency.
Miravitlles M, Dirksen A, Ferrarotti I, Koblizek V, Lange P, Mahadeva R, et al. European Respiratory Society statement: diagnosis and treatment of pulmonary disease in a1-antitrypsin deficiency. Eur Respir J. 2017;50:1700610. doi: 10.1183/13993003.00610-2017.
EARCO: European Alpha-1 Research Collaboration (EARCO) is a pan-European network committed to promoting clinical research and education in alpha-1 antitrypsin deficiency (AATD). The core project is the pan-European AATD Registry, a collaboration which will offer longitudinal real-world data for patients with AATD. EARCO has a global vision to increase the early diagnosis of alpha-1 antitrypsin deficiency (AATD), understand better the natural history of the condition and ensure optimal access to effective care, placing emphasis on ambitions that serve collective needs of the AATD research community and bringing people with AAT deficiency to the centre of the research environment in a real-world context.
Patient support groups
Austria: www.alpha1-oesterreich.at
Belgium: www.alpha1plus.be
Denmark: www.alfa-1.dk
France: www.alpha1-france.org
Germany: www.alpha1-deutschland.org
Ireland: www.alpha1.ie
Italy: www.alfa1at.it
Netherlands: www.alpha-1nederland.nl
Norway: alfa1foreningen.wordpress.com
Poland: www.a1at.wordpress.com
Portugal: www.aa1p.pt
Romania: alfa1romania.ro
Spain: www.alfa1.org.es
Sweden: www.alfa-1.se
Switzerland: www.alpha-1.ch
United Kingdom: www.alpha1.org.uk
Alpha-1 Global
Alpha-1 Global is an initiative by the Alpha-1 Foundation in the USA that provides resources for patients, doctors and scientists: www.alpha-1global.org/en/
The European Lung Foundation (ELF) was founded by the European Respiratory Society (ERS) in 2000 with the aim of bringing together patients, the public and respiratory professionals to positively influence lung health.
This factsheet has been prepared with the assistance of I. Ferrarotti, B. Balbi, M. Miravitlles, T. Greulich and reviewed by patient representatives from Alpha-1 support groups. The factsheet was based on the following article by I. Ferrarotti et al.: Update on a1-antitrypsin deficiency. Breathe 2018 Jun; 14(2): e17–e24. This can be found online at ow.ly/Mr3P30jUEyn
Produced in February 2021.
This page was updated in 2024



If you want to access data on Alpha-1 antitrypsin deficiency in Europe, visit the Lung Facts website
Launched by the International Respiratory Coalition and using data from the Global Burden of Disease study, Lung Facts provides the latest numbers on people living with lung disease by condition and by country.
Learn more




