Sputum: a guide for people with lung conditions
This is a guide about sputum (also known as mucus and phlegm) for people living with lung conditions. It is relevant for anyone who needs to do sputum testing. This could include people living with long-term conditions such as bronchiectasis, chronic obstructive pulmonary disease (COPD), severe asthma, cystic fibrosis, primary ciliary dyskinesia (PCD) or aspergillosis. It could also be for people with short-term infections, such as pneumonia, tuberculosis (TB) or non-tuberculous mycobacteria pulmonary disease (NTM).
Content Table
This guide aims to answer questions about sputum including when and how to take a sputum test and what to do with the results.
This topic can create anxiety, especially if you have been recently diagnosed. The guide aims to inform and reassure you about this topic.
What is sputum?
Sputum, mucus or phlegm are terms used to describe the same thing – the fluid or discharge that comes from the airways in the lungs, also called the bronchi. Normally, the amount of sputum a person produces is very small but for some lung conditions, the amount, colour and consistency of sputum can change.
The amount and appearance of sputum can vary from person to person. The colour can range from white or yellow, to green, dark green or brown.
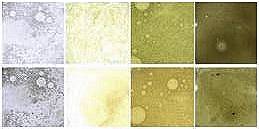 This picture shows different sputum samples from bronchiectasis patients varying in colour from clear to dark green/brown. Sputum can also be multi-coloured and can sometimes include streaks of blood. Some people have darker or bloody sputum when they have a flare-up. Usually, darker sputum means more inflammation in the airways. Some lung conditions can cause sputum to be thicker, stickier or produced in larger amounts.
This picture shows different sputum samples from bronchiectasis patients varying in colour from clear to dark green/brown. Sputum can also be multi-coloured and can sometimes include streaks of blood. Some people have darker or bloody sputum when they have a flare-up. Usually, darker sputum means more inflammation in the airways. Some lung conditions can cause sputum to be thicker, stickier or produced in larger amounts.
These changes can be a normal part of how certain conditions affect the airways. What is most helpful is noticing any change from what is usual for you, particularly if this happens alongside worsening symptoms.
When should you take a sputum sample?
This is different depending on your condition. For bronchiectasis, it is recommended that people should take regular sputum samples each year and when you are ill, for example if you have a flare-up of symptoms (exacerbation) or a chest infection. In cystic fibrosis, a sputum sample is usually sent more often (every 3 months) and when you are ill.
Before any sputum test is performed, it is important to know why your test is needed. There are multiple types of sputum tests, each designed to detect different bacteria or conditions. Your healthcare professional should specify what the test is for when they order it to avoid any errors. The choice of test affects both the procedures performed and the time required for results.
Remember:
Sputum is not saliva – the sputum should come from coughing, not spitting. The sample is tested in a laboratory and the tests can detect whether sputum comes from saliva or lower in the lungs. If the tests see that the sample is saliva, they may not examine it for bacteria.
Storing your sample
If you cannot take your sample straight to a healthcare professional, then keep it refrigerated. It can be kept at room temperature for no more than two hours or in a fridge (not freezer) for up to 18 hours.
How is the sample tested?
Once at the laboratory, your sample will be tested for bacteria and fungi. It is common for one or two bacteria to be found in each sample. When bacteria are found, they will be tested alongside antibiotics to see which is most likely to work. They do this by growing the bacteria alongside different antibiotics to see which ones stop the bacteria from growing. If the bacteria do not grow, it means they are sensitive to that antibiotic and it is more likely to be effective for treatment.
Asking your doctor for something specific
Testing for mycobacteria (a type of bacteria) is recommended in some conditions, for example bronchiectasis. The test is recommended if your condition worsens or before starting long-term treatment with a type of antibiotics called macrolides (such as azithromycin).
Depending on the local laboratory, mycobacteria are not always tested for unless specifically requested.
How do you understand the test results?
Timing of results
Bacteria take time to grow and the timings depends on the specific bacteria and how many bacteria the sample contains. A result may take between two days to a week but in the case of mycobacteria, it can take up to two months due to their slower growth.
Understanding your results
The results will help find out what antibiotics you should be taking to tackle the infection. The information you receive about your results differs depending on the country you live in. In some cases, patients can see their results on an app, in other cases the results will be sent to your local doctor who will contact you.
A report could include:
- The names of the bacteria that have been found and which bacteria could be used to help treat the infection
- The report may include categories for the antibiotics that have been tested including:
- ‘S’ meaning sensitive and could be useful
- ‘R’ meaning resistant to the antibiotic and cannot be used
- ‘I’ meaning intermediate; the antibiotic might work, but it may not be as effective as those labelled “sensitive”.
The report may also contain a number which shows how much of the antibiotic was found to be effective. Using standard guidelines, the laboratory will use this number to say whether the bacteria are sensitive, resistant, or intermediate to that antibiotic.
Example:
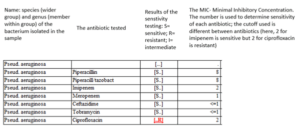
Test results may not perfectly predict how well the antibiotic will work for each person. For example, even if a bacterium is found to be “sensitive” to a certain antibiotic, it may not always be helpful. There are many reasons for this including how the antibiotic reaches your lungs and how your body responds to infection.
The test report is helpful but is not always the only factor for your healthcare team to choose an antibiotic. The choice of antibiotics also depends on other factors, such as whether you are allergic to some antibiotics, have other medical conditions such as kidney disease or whether you are pregnant or breastfeeding.
If the lungs suffer from continuous infections, the bacteria are likely to be found whenever the sputum is tested.
Questions about results
If there is anything you do not understand about the results or the testing process, ask your doctor to explain this to you.
What happens next?
Sputum tests may be used for continuous monitoring and to check for infection. If your infection requires treatment, the decision to take an antibiotic will depend on several factors. This includes:
- Your health: for example, your doctor would likely recommend an antibiotic if you are ill with a flare-up or exacerbation. This would usually be for 10-14 days.
- In some long-term conditions, if a bacterium called “Pseudomonas aeruginosa” grows for the first time. Some doctors will try to prevent these bacteria from becoming a long-term infection by treating with antibiotics.
In some instances, no bacteria are found in a sputum sample during a flare up, and your doctor still treat it with an antibiotic. This is because in some cases bacteria do not always grow in the lab, yet may still be in your airways and cause problems.
Treatment with an antibiotic is started depending on the decision you make with your healthcare team. The sputum test can be a useful resource to guide the decision about if and which antibiotic is given.
Your healthcare team will keep track of your results to help compare them year on year. This is useful for healthcare to look at whether the bacteria found are new or if you have had them before. This tells them whether this is a new or old (recurring) infection.
Where can you find further information?
This document should be used as a general guide to help you understand and prepare for sputum testing. It is important to also discuss the test with your healthcare professional to make sure you feel prepared and informed before sputum tests.
Find out more about different conditions that might need regular sputum testing and other related information:
This information was compiled with the help of members of the ELF patient advisory groups for bronchiectasis, asthma, aspergillosis and COPD and professional expertise from EMBARC. EMBARC is a pan-European network committed to promoting clinical research and education in bronchiectasis, through sharing of protocols, research ideas and expertise.