Bronchiectasis
Bronchiectasis is a long-term lung condition. If you have bronchiectasis, your airways (tubes connecting your windpipe to the lowest part of the lungs) are wider than normal. This leads to mucus (or sputum) building up and making you more at risk of getting lung infections. Infections can cause the lungs to become inflamed, which can damage or block parts of the lung, leading to symptoms like breathlessness, chest pain and tiredness. Bronchiectasis is also known as non-cystic fibrosis (non-CF) bronchiectasis.
Bronchiectasis can occur at any age. This page mainly focuses on bronchiectasis in adulthood.
How do my lungs work?
You have two lungs, which sit on either side of the heart within the ribcage. Each lung is made up of sections called lobes. They are connected to the nose and mouth by the windpipe (trachea).
The lungs’ job is to bring oxygen into the body and to remove carbon dioxide. Oxygen is a gas that provides us with energy, while carbon dioxide is a waste product of the body.
When you breathe in, air passes through a series of connecting tubes (called bronchi or airways) which are designed to take the air towards the bloodstream. The air meets the bloodstream at tiny air sacs called alveoli.
How do my lungs stay clear of infection?
As well as taking air in, the lungs keep unwanted material out of the body. The air is full of small particles and bacteria and the average person inhales nearly one million bacteria per day. However, because the lungs are so effective at getting rid of bacteria, it is rare for people to develop chest infections.
Your airways are lined by a layer of sticky mucus (called sputum when it is coughed up) that traps particles and bacteria, helping to keep the airways moist and clean.
This mucus is constantly being pushed upwards towards the throat so that it can be either coughed up or swallowed. The pushing is done by tiny hairs called cilia which “flick” the mucus upwards. This is the main way that the air passages are kept clean and free of infection.
In bronchiectasis, parts of the lung tubes (airways) become damaged and wider than normal. These wider areas are less effective at clearing mucus (sputum) from the lungs and so mucus gathers and may become infected with bacteria.
Exacerbations may happen when harmful bacteria grow and the body is not able to clear the lungs because of the damage, or because the mucus is too thick.
Research has shown that the airways are never free of bacteria. Studies of samples taken from the airways have found many types of bacteria even in healthy lungs. This is normal and does not require treatment with antibiotics.
Bronchiectasis can affect one, or several parts of the lung. It can be quite mild, where there is not a lot of mucus or can be more severe where people might cough up more mucus.
Infections can cause the lungs to become inflamed, which can damage or block parts of the lung. This can lead to symptoms like coughing up mucus, frequent chest infections, breathlessness, chest pain and tiredness.
What causes bronchiectasis?
Many different things can cause bronchiectasis and it is not always possible to know the cause. In some cases, it can be caused by a bad infection, such as pneumonia or childhood whooping cough. This is called post-infective bronchiectasis. Other conditions that are often linked to or can cause bronchiectasis are:
- The immune system not working properly
- Severe asthma complicated by an allergic reaction to a fungus called Aspergillus – this is called allergic bronchopulmonary aspergillosis (ABPA)
- Conditions where the immune system attacks the body, like rheumatoid arthritis or ulcerative colitis
- An obstruction or blockage of the airways after inhaling something
- Primary ciliary dyskinesia (PCD) – a genetic, long-term condition some people are born with where the lungs do not develop normally
- Chronic obstructive pulmonary disease (COPD) – a long-term condition that causes inflammation in the lungs, damaged lung tissue and a narrowing of the airways, making breathing difficult
- Alpha-1 antitrypsin deficiency – a genetic condition that can cause lung and liver problems
- Tuberculosis (TB) or non-tuberculous mycobacterial (NTM) infections – infections that often affect the lungs caused by the group of bacteria called mycobacteria
Your doctor will ask you some questions and may do some tests to find out why you have bronchiectasis. Often the cause is not found (and is then called idiopathic bronchiectasis). This does not mean that there is no cause, just that it is not known. The basic treatment of bronchiectasis is usually the same, no matter the cause. However, some causes call for a particular type of additional treatment.
How is bronchiectasis diagnosed?
The common symptoms of bronchiectasis are having a cough that is hard to get rid of, coughing up mucus, being short of breath and getting lots of lung infections. These symptoms are seen in other more common lung conditions like COPD or asthma, so most people are tested for them first. However, it is possible to have two, or even all three, of these conditions at the same time. If your healthcare professional thinks you have bronchiectasis, they will do some extra tests.
Common first tests
Chest X-ray: bronchiectasis cannot usually be seen in an X-ray, but it can help rule out other conditions.
Spirometry: this is a breathing test that involves blowing hard and fast into a machine, emptying the lungs of air. It will not diagnose bronchiectasis, but is one way of measuring whether the lungs are damaged.
Sputum samples: your doctor or nurse may ask you to cough some sputum into a container for testing in a laboratory. This can identify bacteria in the lungs, in order to find the best antibiotic to use if you have a chest infection.
Blood test: this can help to check your general health.
Specialist tests
CT (computed tomography) scan: this test is needed to diagnose bronchiectasis. This is where you receive low-dose X-rays at a number of angles before a computer puts together a detailed image.
Tests of the immune system: your doctor might organise blood tests to check how your immune system works and to check for possible causes of bronchiectasis, such as a lack of antibodies that fight infection or severe allergies.
Breathing tests: spirometry (see above) may be performed, along with other more detailed lung function tests.
Depending on your symptoms you may have further specialist tests to try to understand the cause of your bronchiectasis. For example, tests for primary ciliary dyskinesia.
What are the symptoms of bronchiectasis?
Each person’s experience is different, so it is not possible to describe a typical person with bronchiectasis. However, you will have some or all the following symptoms:
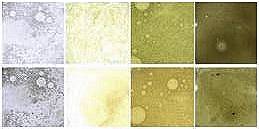
- Cough – which often involves coughing up mucus (sputum). The amount of sputum coughed up can vary a lot, as can the colour (which may be white, yellow, green, dark green or brown as shown in the below image).
- Breathlessness – caused by the damaged airways working less well. In many cases, breathlessness is not a problem, but sometimes people may notice they are out of breath when walking uphill or up stairs. In severe cases, people may get breathless during less strenuous exercise.
- Feeling very tired – the body uses a lot of energy to fight infections, as well as to cough and breathe. This can be made worse if people have trouble sleeping due to other symptoms.
- Chest discomfort – this can be a pain, tightness or a feeling of ‘fullness’ in the chest.
- Exacerbations or worsening of symptoms for periods of time – you might easily catch infections that more quickly affect your chest. Other symptoms may get worse during an exacerbation. Find out more in the ‘exacerbation management’ section.
If properly treated and monitored, most people with bronchiectasis have a normal life expectancy. People with bronchiectasis are more likely to die because of other medical conditions that affect all people (like heart disease or cancer) than to die directly from bronchiectasis.
How severe is my condition?
Bronchiectasis is a complicated condition and there is not one single test or sign of whether your condition is mild, moderate or severe. However, if your bronchiectasis is well controlled you should have few symptoms and be able to lead a normal life.
Your bronchiectasis will be considered to be more severe when symptoms start to affect daily activities.
Factors linked with more severe bronchiectasis include:
- Breathlessness: being unable to walk 100 metres without stopping.
- Exacerbations: having three or more in a year.
- Regularly growing bacteria on mucus (sputum) samples: this suggests your lungs have some regular infection, particularly if a bug called Pseudomonas is regularly found.
- If both lungs or several parts of the lung are shown to be affected on a CT scan, rather than a small part of the lung.
- Hospital admissions: if you have had to go to hospital with a bad chest or because you needed antibiotic injections.
- Weight loss: if having bronchiectasis causes you to become underweight.
- Lung function tests: having lower lung capacity.
- Getting older: can impact on symptoms and severity of bronchiectasis.
These are only a guide – some people may have several of these and still live a normal life; while some people may have none of the above, but have other important factors that cause them to feel more unwell. Many of these factors can improve with effective treatment.
People with severe bronchiectasis are at risk of a reduced life expectancy, which is why they should do everything they can to keep their lungs healthy.
How long will I live?
For patients with mild/well controlled bronchiectasis there should be no difference in life expectancy than the population as a whole. For patients with severe/uncontrolled bronchiectasis or with additional risk factors the importance of good control is very important as there may be an impact on life expectancy.
Do also discuss your own condition with your consultant or doctor if you want to know more.
Links with other conditions and infections
People with bronchiectasis may also have other medical problems and conditions such as:
- Rheumatoid arthritis or an immune system problem.
- Sinusitis can be caused by the same problems as bronchiectasis.
- Conditions that have no relationship to the bronchiectasis.
These additional problems can have an impact on your quality of life. It is important to be aware that treatments for bronchiectasis might interact with treatments for other conditions, which cause side effects. If you are seeing a doctor or nurse for another condition, always make sure they know you have bronchiectasis and are aware of the treatments you are taking.
Some other conditions might make the symptoms of bronchiectasis worse. For example, inflammation of the nose (rhinosinusitis), symptoms of asthma, allergies, reflux from the stomach or problems with the immune system. Your doctor will treat these problems as well as treating your bronchiectasis to try and improve your condition.
-
The difference between bronchiectasis, COPD and asthma
Bronchiectasis, asthma and COPD (chronic obstructive pulmonary disorder) are 3 different conditions that are treated in slightly different ways. They can cause very similar symptoms and so there is sometimes confusion between them.
It is possible for individuals to have two of these conditions or even all three.
COPD is usually caused by cigarette smoking, whereas bronchiectasis and asthma are not caused by smoking. Asthma is a condition where the airways become inflamed, often associated with allergies.
COPD and asthma are more common than bronchiectasis and are usually diagnosed based on the symptoms and lung tests. It is not possible to diagnose asthma or COPD on a CT scan.
-
What is bronchopulmonary aspergillosis?
Bronchiectasis can be caused by a bad allergy to a fungus that is found everywhere in the environment called Aspergillus or other fungi. The immune system responds in an overly aggressive way to this fungus, causing damage to the lungs and symptoms that are like an asthma attack. This is called allergic bronchopulmonary aspergillosis (ABPA for short). Individuals with this condition often have a history of asthma in the past.
The treatment for this condition is to dampen down the immune system with steroid tablets or other drugs that prevent inflammation. Sometimes, antifungal tablets (like antibiotics but that work specifically against fungi) are also added to help reduce the reliance on steroid tablets.
If bronchiectasis has developed, the damage is often not reversible, and so after the ABPA has been successfully treated, you will need treatment for the bronchiectasis over the long term.
-
What is NTM (non-tuberculous mycobacteria)?
Non-tuberculous mycobacteria (NTM) refers to a group of bacteria from the same family as tuberculosis (TB) but which cause a different kind of infection than TB.
NTM live in the environment and rarely cause any problems for people without lung disease. However, NTM can infect areas of the lung that have been damaged or infect people who have problems with their immune system. There are many different types of NTM causing many different types of disease.
The typical symptoms of NTM infection in the lungs are cough, tiredness, weight loss, breathlessness, and sometimes chest pain or coughing up blood.
NTM pulmonary disease can be a cause of bronchiectasis, where someone can pick up the bug and the bug causes damage to the lungs resulting in bronchiectasis. However, there is no agreement on this always being the case, and bronchiectasis may instead act as a cause of NTM pulmonary disease. It is also possible for NTM to infect the lungs in people that already have bronchiectasis, and this can cause symptoms to get worse.
NTM do not damage the lungs in the way that TB does, and sometimes people live with NTM in the lungs without needing to take any extra treatment because the effects are quite mild. The treatment of NTM involves a prolonged course of antibiotics.
Unlike tuberculosis, NTM is in most cases not contagious, and a person with NTM does not need to be in isolation.
Visit NTMinfo.org where there is very good information about NTM available including a brochure in 8 languages.
-
What is Pseudomonas?
Pseudomonas aeruginosa, or Pseudomonas, is a bacterium (or ‘bug’) that can cause infection in people with bronchiectasis. It affects about 1 in 5 of those with bronchiectasis at some point.
It is found everywhere, in soil, water, on the skin of some people and in most man-made environments. It does not usually cause infection in healthy people, but it can infect damaged lungs such as those in bronchiectasis.If you catch Pseudomonas, your doctor may recommend a course of antibiotics to try to get rid of or to control it, or they may recommend that you take a different antibiotic when you get chest infections in the future.
People with Pseudomonas can sometimes have more chest infections and more problems than other people with bronchiectasis because of its resistance to antibiotics, and sometimes it can damage the lung. Guidelines for doctors therefore suggest that people with Pseudomonas are monitored more regularly.
How is bronchiectasis treated?
Treatment for people with bronchiectasis has several aims:
- To prevent chest infections (exacerbations), during which symptoms get worse
- To treat symptoms
- To improve quality of life
- To stop the condition from getting worse
With good treatment, it is possible for people with bronchiectasis to remain stable for many years and to have good control of their symptoms. The following are some of the commonly used treatments for bronchiectasis, including those recommended to doctors as part of the European bronchiectasis guidelines. Not all of these treatments are available or used in all European countries. If you have any questions regarding these treatments, please discuss them with your doctor.
The disease progresses through what is called a ‘vicious cycle’ of infection, inflammation and lung damage. Infections cause the lungs to become inflamed and the inflammation damages the lung. More lung damage makes you more susceptible to infection. We can tackle all three aspects of the cycle as shown in the diagram:

Treatment for inflammation
- Inhalers: some inhalers contain medicine that opens up the airways to make it easier to breathe and reduce inflammation in the lungs.
- Tablets: some medications can also reduce inflammation. This includes a type of antibiotic called macrolides, which can reduce inflammation as well as treat infection.
- Other strategies to improve inflammation are currently being developed.
Treatment for lung damage
- Physiotherapy and airway clearance exercises can help to clear mucus.
- Medications can help to clear mucus (mucoactive drugs). These should be combined with regular physiotherapy exercises to be most effective.
- Bronchodilator inhalers relax the muscles in the airway.
- Regular exercise helps to clear sputum and encourages the lungs to work better.
- Other important considerations are to avoid smoking and to treat the underlying cause of bronchiectasis if this has been identified.
Treatment for infection
- Vaccines: having an annual flu vaccine and a pneumococcal vaccine (which protects against the most common bacterial cause of pneumonia) is important to lower the risk of getting these infections.
- Antibiotics: any chest infections should be treated quickly with antibiotics – taken as tablets, through a mask (nebuliser) or as injections.
- Preventative antibiotics (in some cases): if you get lots of chest infections or have very severe symptoms, you may be given long-term antibiotic treatment to suppress the bacteria in the lungs. The doses are lower than those given to treat an infection, and are often given for at least 1 year and sometimes longer. They will not work straight away and need to be taken regularly to have their full effect. These medications can interact with other tablets, so it is important to tell other doctors that you are taking regular antibiotics before they prescribe you other drugs.
- Clearance of bacteria like Pseudomonas: Pseudomonas aeruginosa, or Pseudomonas, is a bug that can cause infection in people with bronchiectasis. If you have Pseudomonas your doctor may recommend a course of antibiotics to try to get rid of or control it, or that you take a different antibiotic when you get chest infections in the future. People with Pseudomonas can sometimes have more chest infections and complications because of its resistance to antibiotics, and sometimes it can damage the lung. Guidelines for doctors recommend that people with Pseudomonas are monitored more regularly.
What are antibiotics?
Antibiotics are a group of drugs that fight bacterial infection. They can be given by mouth (oral) as tablets or liquid, or by injection (intravenous, which means directly into the vein). Some antibiotics can be put into a nebuliser to be taken regularly (inhaled). Different antibiotics work against different bacteria, but many work against multiple bacteria.
Common oral antibiotics that are used in treating bronchiectasis include:
• Penicillins: these include penicillin, amoxicillin and coamoxiclav (amoxicillin-clavulanic acid)
• Macrolide antibiotics: these include clarithromycin, erythromycin and azithromycin
• Doxycycline: this is another type of antibiotic taken once a day
• Quinolones: these include ciprofloxacin, levofloxacin and moxifloxacin and are the only medications taken by mouth with activity against Pseudomonas infection.
Antibiotics can either be taken for a short period of time (days) to treat an exacerbation caused or aggravated by bacteria, or long-term (months and years) to prevent exacerbations.
The most commonly used long-term antibiotics are macrolides like azithromycin, clarithromycin, erythromycin and roxithromycin. They can be taken every day, or sometimes three times per week. The doses are lower than those given to treat a full blown infection, which helps to reduce the side effects.
Nevertheless, up to 1 in 5 people with bronchiectasis will get some side effects; most often diarrhoea or abdominal pain. Tinnitus (ringing in the ears) is a rare side effect but you should stop taking the medicine if this happens and speak to your doctor. These medications can interact with other tablets and so it is important to always tell other doctors that you are taking regular antibiotics before they prescribe you other drugs.
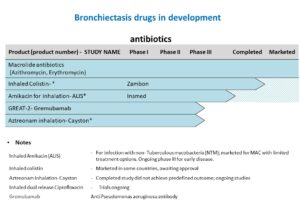
Drugs in development
Developing medications is a structured and regulated process. It usually begins with an idea that a certain compound could benefit patients by improving their condition.
The compound is first tested in the laboratory – in cells or animals – to find out if it could be beneficial. Only then is the compound tested in humans, in a series of studies called “clinical trials”. If these prove safe and effective, the compound may then be licensed and marketed as a drug for treatment of the condition. Clinical trials are usually conducted by drug companies, but in some cases by academic institutions.
-
Clinical trial phases
Clinical trials are tightly regulated by laws, which were made to protect participants, while ensuring that the drug in development will not be released for use as a patient treatment until it is safe and effective.
These trials are advanced in steps, each of which has to be successful in order to move on to the next phase – see phases I to IV below:
- Phase I trials determine how safe a compound is in healthy volunteers (looking out for potential undesired side effects).
- Phase II trials determine safety and the optimal dose in patients (the amount of the compound and how often it should be taken).
- Phase III trials determine the compound’s effectiveness in patients.
- Phase IV trials may be performed after the drug is already licensed and usually look for the effect of the drug outside the limited specifications of earlier clinical phase trials.
Each phase trial must show that it was successful in order to move on to the next phase trial.
Due to the complexity of these processes, it typically takes years from early development to marketing of a drug. In this process, many compounds fail to demonstrate effectiveness or for other reasons their development may be stopped.More information on how drugs are developed may be found in EUPATI- European Patients’ Academy
-
Clinical trials registration
By law, clinical trials must be registered before recruiting participants.
Examples of such registration sites are the US National Institutes of Health (NIH) “clinical trials” or the European “EUDRACT” and these are available to search by professionals and the public.
-
Drugs used to treat people with bronchiectasis
In bronchiectasis, many drugs are used although they were developed for a different use (indication).
One example is Colistin – an antibiotic that was developed for use as an intravenous antibiotic – but is commonly used for long-term inhalation in bronchiectasis.
Such use is sometimes referred to as off-label, meaning that it is used differently from the original registration.
Drug compounds in development
For more information on how you could help with research and clinical trials, visit the ‘How we work together with patients and care givers’ page or check out our programme on how to become a patient ambassador:
Antibiotics (Drugs that are active against bacteria)
- Inhaled Amikacin (ALIS) – For infection with non-Tuberculous mycobacteria (NTM); marketed (USA) and ongoing
- Inhaled Colistin – Marketed in some countries, other phase III studies ongoing
- Aztreonam inhalation – Cayston – Completed study did not achieve predefined outcome; phase II to begin
- Inhaled dual release Ciprofloxacin – Trials ongoing
- Inhaled dry powder Tobramycin – Phase II completed
Drugs that target inflammation
Inhaled A1AT – a protease inhibitor – A1AT- alpha 1 antitrypsin
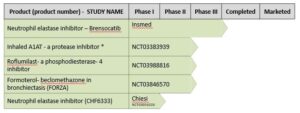
Other drugs
Hypertonic saline – Use as physiotherapy adjunct
Inhaled mannitol – Phase III completed
ENaC inhibitor for patients with PCD (VX 371) – CLEAN-PCD – For PCD- Primary ciliary dyskinesia, a specific cause of bronchiectasis

Other types of treatment
Oxygen therapy
If your oxygen levels are low, you may need to breathe oxygen in through a tube or a mask. This could be short term (e.g. when you are in hospital with a chest infection until your levels return to normal) or long term if your lung has been damaged and is no longer able to take in enough oxygen. You may also need additional oxygen during flights. Speak to your healthcare professional about this before you travel.
Surgery
In most cases bronchiectasis can be well controlled and cared for without surgery. Surgery can sometimes be helpful if bronchiectasis affects only a small part of the lung and so might be cured by removing it, or if a section of the lung has been very badly damaged and is causing a lot of infections.
Pulmonary rehabilitation
You may be offered pulmonary rehabilitation as a way of improving your physical strength and reducing the impact of symptoms on your life. Pulmonary rehabilitation is a type of treatment that aims to reduce the physical and emotional impacts of a lung condition on a person’s life. It is a personalised programme that combines exercise training with education about ways you can help keep yourself as healthy as possible.
Support to stop smoking
Smoking does not cause bronchiectasis, but it can make your condition and symptoms much worse. There is help available for you to stop smoking and alternatives to make quitting easier. Talk to your healthcare professional about how they can support you.
Self-management
Self-management is very important for people with long-term conditions like bronchiectasis. There is a range of different things you can do day-to-day to manage your condition. These include taking your medications and doing airway clearance exercises as recommended; monitoring your symptoms and telling your healthcare professional about any changes; being physically active; eating healthy foods; and, if you smoke, stopping smoking.
Clearing mucus from the lungs
Bronchiectasis leads to a build-up of mucus which can make infections more likely and also causes worsening symptoms of cough and breathlessness. It is therefore essential that you learn to clear mucus from the airways effectively. This is done by:
Taking medication to help clear the lungs (mucoactive drugs): Some medications are given by a nebuliser or might be given by an inhaler or tablet and are designed to help the mucus come up more easily. For example, inhaling salt water solutions from a pharmacy (saline) helps to hydrate mucus making it less thick and therefore easier to cough up. Other drugs which try to do similar things include mannitol (given via an inhaler) and carbocisteine (which is taken as tablets).
These medications should be combined with regular physiotherapy exercises for the best effect. It is also important to keep hydrated as this helps loosen the mucus.
Keeping your chest clear of mucus (sputum):
Everyone with bronchiectasis should see a respiratory physiotherapist to be shown how to use chest clearance techniques. Ask your doctor to refer you.
A physiotherapist will assess you and examine your chest. They will discuss which methods can help you remove mucus (sputum) from your lungs and help you choose the best techniques for you. These are called Airway Clearance Techniques.
It is very important to clear your chest of as much sputum as possible to help reduce the number of chest infections that you have. The techniques shown below will help to reduce the obstruction in your airways, improve the amount of air getting into your lungs and help to reduce bacterial infections.
“The most important skill you can learn is lung clearance. No matter how tired you are, lung clearance needs to be done and if you are going out, arrange lung clearance around it so you can still enjoy yourself” Sue, individual with bronchiectasis, UK
Airway clearance techniques
-
Active cycle of breathing
There are 3 parts to this technique:
- Breathing control
- Deep breathing, also called Thoracic Expansion Exercises (TEE)
- Huffing, also called Forced Expiration Technique (FET)
-
PEPs e.g. Flutter or Acapella
PEPs (positive expiratory pressure) are hand-held devices to help clear your sputum. Common trade names are the Flutter and Acapella.
You breathe out through the device against a slight resistance which creates oscillations (flutters) in the pressure of your airways.
This prevents the airways from collapsing and loosens sputum. You need to be assessed to see whether this device is suitable for you.
-
Autogenic drainage
This is a breathing exercise that involves breathing out as far as possible to loosen any sputum from the small airways at the edges of your lungs. The sputum can then be moved to the more central airways making it easier to cough up.
-
Postural drainage
This is a chest clearance technique that involves moving into different positions that help mucus to drain from different parts of the lung.
It is often combined with percussion where gently clapping on parts of the body helps to move mucus from the farthest away parts of the lung into the central airway tubes where it can be easily coughed up.
Specialist care
Treatment of bronchiectasis is best provided by a team of healthcare professionals that are experienced with the condition. In many countries there are now specialised clinics dedicated to people with bronchiectasis.
These clinics will all be slightly different but may include:
- A doctor, or team of doctors, with a specialist interest and experience in bronchiectasis
- A physiotherapist, or team of physiotherapists, that can teach chest clearance exercises
- Nurses or other healthcare professionals that can provide education and support
- Services to provide inhaled/nebulised antibiotics, other specialised medications and intravenous antibiotics at home
- Specialised tests of the immune system or body to diagnose the cause of bronchiectasis
Some people with bronchiectasis regularly attend specialist clinics, while some might go once, or on a few occasions, and then be transferred back to the care of their regular doctor.
If you think you need to see a specialist, please discuss this with your doctor. There is no directory of bronchiectasis specialists across Europe, but if you have difficulty finding one, please contact us.
What to expect from specialist care: patient checklist
The Bronchiectasis Patient Checklist is based on the European Bronchiectasis Guidelines 2017 and reflect what most patients with bronchiectasis should expect from their care according to these guidelines. Ask your specialist, doctor or nurse to go through the checklist. You can keep track of each recommendation by ticking it off the checklist.
What you can do: managing bronchiectasis
There is a lot you can do to help manage your condition alongside treatment prescribed from your doctor. The skills and techniques outlined here are very important to learn to make sure you keep as well as you can.
Download our self-care guide written by people with bronchiectasis. This printable document aims to give you an overview of how to live a full life with the condition.
Look after yourself
It is good advice for people with bronchiectasis to look after their general health. Eat a healthy balanced diet and take regular physical exercise. Dehydration can make mucus thicker and harder to clear and so you should stay well hydrated.
Remember to take your medications as prescribed and get the annual influenza vaccination, COVID-19 vaccinations if available as well as the periodic pneumococcal vaccination.
As people with bronchiectasis are at higher risk of picking up infections, it is a good idea to wash your hands before eating, but also before preparing medications, performing chest clearance or any other medical procedures e.g. cleaning nebulisers.
Keeping active
Try to do some exercise every day.
Exercising and keeping active can help clear mucus from your lungs and can often give you more energy and help you sleep better.
It has been proven that working the lungs through exercise actually improves breathlessness and reduces tiredness. Talk to your doctor or physiotherapist about the best exercise for you and try to do some every day, building up gradually.
Find out more about pulmonary rehabilitation.
Coping with fatigue
It is common to feel very tired when you have bronchiectasis. You may find this tiredness, or fatigue, overwhelming and leave you with little energy for everyday tasks.
Fatigue affects everyone differently but you may:
- Have general lack of energy.
- Find it hard to concentrate or make decisions.
- Feel irritable and get upset easily.
- Have difficulty remembering things.
- Have interrupted sleep.
- Withdraw from family and friends
Tips for conserving energy
- Use breathing control techniques regularly and maintain good posture.
- Save energy e.g. let dishes air-dry; sit for as many activities as possible.
- Maintain a regular programme of gentle exercise.
- Pace yourself by giving yourself more time to do things and plan rest periods.
- Organise your time – do most energy consuming tasks at the time of day/week when you have most energy.
- Get assistance – do not be afraid to ask for help.
- Organise your space – put the items you use most in drawers or shelves that are between waist/shoulder level.
- Try to get good-quality sleep.
- Eat a well-balanced diet and drink plenty of clear non-alcoholic fluids.
- Relax.
Coping with breathlessness
Your physiotherapist can advise on how to manage your breathlessness.
Most people get breathless from time to time, for example when they exercise or run for a bus. This passes quickly and should not be too uncomfortable.
However, some people with bronchiectasis can get breathless very easily. This breathlessness tends to be uncomfortable, severe and can come on with very little exertion. It can also make you feel very anxious.
-
What can help with breathlessness?
Learning to control your breathing will help you to control your breathlessness and reduce any feelings of panic and anxiety.
Your physiotherapist will advise on how to manage your breathlessness which may include:
- breathing control techniques
- different positions to relieve your breathlessness
- what exercise you can do
- techniques to conserve your energy and pace yourself
- relaxation techniques
-
Be prepared
Being prepared for breathlessness can help to reassure you when it happens and lessen your anxiety:
- If you get breathless, or wake up breathless, sit up and lean forward e.g. sit at the edge of a seat/bed and lean your arms on a table.
- Using a fan can help some people.
- Keep your inhalers handy and take your reliever.
- Try to use your breathing control techniques.
- Try not to fight it and relax your shoulders.
- If the breathlessness is new or worse, see your doctor.
Coping with low mood and depression
Feeling down for some of the time is a natural reaction as you learn to accept, and adapt to, your condition. Read our information on mental wellbeing and lung health for more advice on this.
“I think forums are invaluable, not only for information but for support from people who really ‘get it’. Sue, individual with bronchiectasis, UK
Exacerbation management
An exacerbation is also sometimes called a chest infection or a “flare up” of bronchiectasis.
Download our flowchart with information about how to recognise an exacerbation and what steps to take.
Incontinence
Coughing can sometimes cause incontinence in men and women. This can include accidental weeing or pelvic floor prolapse (when one of the organs in the pelvis slips down causing discomfort). If this happens, it’s important to seek a referral to a physiotherapist to help manage these symptoms.
Sex and relationships
Keep communicating and sharing your feelings with your partner.
Bronchiectasis does not affect your sexual ability but some associated problems can cause issues. Lack of energy, coughing and breathlessness may affect your stamina, interest in sex and lead to avoidance of sexual intimacy. This can also be a worry when you start a new relationship.
Depression and anxiety can also have an effect on your sex drive. Your partner may feel it is better to avoid sex as they do not want to upset you. It is important to keep communicating honestly with each other as maintaining intimacy and closeness can help to combat any loneliness and isolation you may feel.
Talk to your partner about how you feel and any worries you may have. This will make it easier for you to deal with the situation before it becomes a problem.
-
Sex and relationships: top tips
You may find these tips helpful but if you have any questions regarding your sexual relationship talk to your doctor. They will be used to talking about personal matters so try not to feel embarrassed.
- Think of sex as another form of physical activity and plan when to have sex.
- Clear any chest secretions using your chest clearance techniques before sex.
- Use breathing control as you would with any other activity and have rests as necessary.
- Choose a position that is less energetic and avoids pressure on the chest e.g. lying on your side during intercourse may be more comfortable and less tiring.
- Do not make love if you are tired at the end of the day. Choose a time of day when you feel at your most refreshed and relaxed.
Travelling with bronchiectasis
A bronchiectasis diagnosis does not mean you have to give up travel, whether on holiday or for business. You just have to think ahead about fitting your normal medication and physiotherapy into your travel schedule. Talk to your doctor and plan it together.
This information is based on ‘Recommendations for travelling with bronchiectasis: a joint ELF/EMBARC/ERN-Lung collaboration‘ and supplemented by tips from travellers with bronchiectasis.
-
Is it safe for most people with bronchiectasis to travel?
It is safe for most people to travel with bronchiectasis. If your condition is stable and you are not feeling unwell then you are likely to have no problems with flying. However, you may still need to seek your doctor’s advice before planning or booking a flight.
Consult your doctor if:
- You feel you may be getting an infection.
- You have had recent bouts of being unwell.
- You are in any doubt.
Sometimes, it may be better to postpone your trip.
You will need medical clearance to fly if:
- Your fitness is in doubt as a result of a recent illness, a period in hospital, surgery or you have a condition that is unstable.
- You need any special service or equipment e.g. assistance, oxygen.
Some people, though certainly not all, find they experience more exacerbations when travelling frequently. If considering a job or career requiring frequent travel, you may want to consult your specialist doctor.
-
Are there any destinations or conditions I should avoid?
You need to take care with:
- High altitude – lower oxygen levels may cause problems for some. You can still enjoy the mountains, but be wary of going too high, and too quickly. Follow recommendations for avoiding altitude sickness and do consult your doctor if you plan on going above 3050 metres (10 000 feet).
- Cities with heavy air pollution – fine to pass through but inadvisable to stay. Check air pollution levels for individual cities on Air Pollution in the World – Real-Time Air Quality Index.
-
What medications should I take?
Pack your regular medications – just make sure:
- It is all in your hand luggage in case of delays or your hold-luggage gets lost.
- It is all in its original containers, backed up by a copy of your prescription, in case you are asked about it at a security check.
- You have enough for your length of trip plus extra in case of unexpected delays on your return.
- If your medication needs special storage conditions, check these are available in your destination.
- If you are crossing several time-zones, ask your doctor or pharmacist for advice about adjusting when you take your medication.
‘Rescue pack’:
Your doctor may also prescribe a ‘rescue pack’ of stronger medication to tide you over in case you pick up an infection while you are away. Ask them:
- How to recognise when to take it.
- When/where to seek local medical help if you get worse.
If you use a nebuliser:
- Ask your doctor or physiotherapist about lighter, portable models.
- Practise using and cleaning it before you go and take spare batteries or a plug adapter.
- If it works on mains electricity, check the voltage in your destination. European nebulisers (220-230V) may not work on lower voltages, e.g. in USA or Canada (120V) – check voltages on www.worldstandards.eu
- If flying, try to nebulise in the airport before and/or after the flight rather than on the plane if at all possible.
A couple more things you need to do:
- Check that any general medications recommended for your destination (such as malaria tablets) do not clash with your regular treatments.
- Make sure that you are up to date with flu jabs/shots and a pneumonia vaccination (also known as pneumococcal vaccine).
And don’t forget everyday hygiene to guard against other people’s colds/flu/other infections:
- Wash your hands frequently.
- Use hand sanitiser – have a little bottle in your pocket at all times.
- Consider using face masks in public places (especially planes and public transportation), but don’t share things like towels, pillows, drinking bottles/cups, sunglasses, cutlery or earphones. You need to take care with:
- High altitude – lower oxygen levels may cause problems for some. You can still enjoy the mountains, but be wary of going too high, and too quickly. Follow recommendations for avoiding altitude sickness and do consult your doctor if you plan on going above 3050 metres (10 000 feet).
- Cities with heavy air pollution – fine to pass through but inadvisable to stay. Check air pollution levels for individual cities on Air Pollution in the World – Real-Time Air Quality Index.
-
Should I take any documents about my condition?
If your bronchiectasis is stable and you are managing it well:
- Check the regulations about prescription medications wherever you are travelling. Some medications may only be allowed in certain amounts, or require documentation, or may be illegal in some countries – check with the embassy of the country you are going to.
- Take a copy of the prescriptions for your regular medications.
- Carry a letter from your doctor stating the purpose of the medication.
Excess hand baggage is usually allowed for medical devices, including a nebuliser, physiotherapy device, oxygen equipment or bulky medications. In this case, again:
- Make sure you have a doctor’s letter about your condition.
- Take a copy of your prescription or other supporting documentation.
If you’ve recently been ill, or prone to frequent infections, ask your doctor for a Medical Report for Treatment Abroad (PDF), to guide medical staff in case you need treatment. This should include:
- Your health status, allergies, chronic infections, regular medications and devices.
- Your recommended treatment for an exacerbation or sudden worsening of your condition.
-
What about chest clearance while I am travelling?
Plan ahead, adapt and improvise:
- Before you go, ask your physiotherapist about clearance techniques that can be done say, in a public toilet, without help or equipment.
- Try to clear your chest before and after a flight or long bus/train journey.
- If you use a saline nebuliser, on a long-haul flight you may have to use it in your seat and then do your clearance in the toilet to avoid disturbing other passengers.
- Take plenty of tissues (plus plastic bags for their disposal – nappy bags are ideal!).
- Avoid taking cough suppressants, they are not recommended for bronchiectasis.
If you are on a busy guided tour, you may want to tell the tour manager you will need enough time and space to use your nebuliser and/or do physiotherapy.
-
What travel insurance do I need?
First, you must tell your travel insurer that you have bronchiectasis. They will ask you a series of questions to ascertain the level of risk – such as ‘Have you been hospitalised in the past year?’, ‘How far can you walk without becoming breathless?’/
Then make sure you have a policy that covers you for:
- A pre-existing chronic condition (bronchiectasis).
- Medical treatment in case that condition worsens while you are abroad.
- Getting home in a severe health emergency.
-
What if I need extra oxygen during a flight?
Most people with bronchiectasis don’t need this but check with your doctor well in advance to see if your lung capacity or oxygen uptake is especially low.
If they say you may need oxygen during the flight, you will need extra documentation and you should let the airline know.
If you are already using oxygen, then still let the airline know, and you may need to turn it up in flight.
Information about air travel for people with all chronic lung conditions can be found in the air travel section of this website. It includes information on airline oxygen policies and contact details as well as details of oxygen providers in other countries.
-
Will it limit my activities on holiday?
No more than at home.
One sport where you will need to exercise caution is SCUBA diving. This depends on your condition – changes in depth may cause air trapped behind phlegm to expand and cause damage to your lungs. Diving may be safe if:
- You have no sputum, shortness of breath or cysts, and,
- Your lung function is normal.
If you are not sure, consult your speciality clinic. Otherwise, stick to a snorkel.
Whatever you are doing outdoors it is best to use high-strength sunscreen as certain treatments can increase your skin’s sensitivity. Also drink plenty of water to keep hydrated.
If you are physically able, then you walk, run, cycle, swim, ski or whatever you fancy. Just take the conditions into account and don’t overdo it. Or be lazy – it’s your holiday.
Happy travelling!
FAQs
-
What is sputum?
The average person inhales 1 million bacteria each day as well as dust and other particles from the environment. As a result, the lungs have developed methods for keeping the lungs clear of infection and getting rid of unwanted particles. Mucus is made by special glands in the lungs and lines the lung tubes. When something is inhaled, it is trapped by the mucus so that it cannot travel further in the lungs, and special hairs called cilia “flick” the mucus up towards the mouth where it can be cleared. This happens in healthy people as well as people with chest conditions. When mucus is coughed up, it is called “sputum”.
In people with bronchiectasis the glands make more mucus, and the mucus can be thicker and stickier than usual because of inflammation in the lungs. The cilia hairs cannot clear all of the mucus. The mucus builds and so has to be coughed up from the lungs.
-
How do I collect sputum samples and how quickly should I send samples off?
It is very useful to have sputum samples for testing in order to know if there is infection in the lungs. This can help your doctor decide what antibiotic to give in the event of a chest infection, and can also detect some bacteria that need to be treated differently, like Pseudomonas or non-tuberculous Mycobacteria (NTM).
It is important therefore that the samples you provide have come from the lungs. They should be coughed up, rather than from clearing the throat or containing mostly saliva. Ideally, wash the mouth out with water before coughing up a sample as this will help to get rid of saliva and cells from your mouth. Cough or spit the sample directly into a pot or container that your doctor or nurse has given you for the sputum. Samples from tissues or that have touched another object before going into the container will not be useful as they could pick up bacteria from the environment.
Once you have a sample, deliver it straight away to your doctor or whoever requested the sample. Bugs start to die once they are outside the body and so within a few hours the chances of getting a positive test from the sputum go down quite quickly. Therefore, try to give them the sample as soon as possible after coughing it up, and certainly on the same day as it was coughed up.
-
What happens when I send sputum samples?
It is important to send sputum samples to the laboratory, even when you feel well, so that your doctor can see whether you have infection growing in the lungs. This helps to decide the best antibiotics to use if you develop chest infections in the future. The test is more likely to be positive with a good sample from the lungs. Saliva will not usually have a lot of bacteria in it. A positive test suggests that there is infection in the lungs, but this does not necessarily need to be treated with antibiotics.
When you send a sputum sample, it gets taken to a microbiology laboratory where a small amount is taken away and put on a plate to grow. Any bacteria present in the sample will grow over 24 to 48 hours and so the microbiologist will then be able to tell what bacteria were present in the sample.
The bacteria can then be tested against different antibiotics, by seeing if they can grow in the presence of different amounts of antibiotics. This process takes another day or two.
This is why is takes a few days to get the final results of your sputum test, because the microbiologist has to identify the bug, and also find out what antibiotics will kill it.
-
Can I pass on infections to others?
Bacterial infections
Many people with bronchiectasis have infections in their lungs caused by bacteria. The bacteria live in the lungs and do not go away completely, even with antibiotic treatment. Where these bacteria come from is usually not known. Everyone has bacteria that live in their nose and throat and so it is likely a lot of the bacteria in the lungs travel down from the nose and throat.
Bacteria like Pseudomonas and Haemophilus that are the most common bacteria in bronchiectasis do not cause infections in healthy people. They are only able to cause infections in bronchiectasis because of the damaged areas of lung that let them survive in the lung. There is therefore no evidence that you can pass on infections to people without bronchiectasis.
There is also no evidence that people with bronchiectasis can catch bacteria from other people with bronchiectasis. It is not possible to say that it could never happen, as in cystic fibrosis , an inherited form of bronchiectasis, it has been shown that some bacteria like Pseudomonas can be passed from one person with cystic fibrosis to another on rare occasions. As a result, it is recommended that people with cystic fibrosis are segregated (they do not sit next to each other in clinics) and do not meet socially or in patient support groups.
Bronchiectasis is usually associated with less severe lung disease than cystic fibrosis and bacteria like Pseudomonas are less common. It is therefore not currently recommended that people with bronchiectasis be segregated and individuals should feel free to attend patient support groups, pulmonary rehabilitation classes and other events where they mix with other people with bronchiectasis. If you are invited to an event, like a pulmonary rehabilitation class, where you would mix with other people with bronchiectasis, you should consider the information above and come to your own decision about whether a theoretical risk of catching an infection would outweigh the benefits of treatment and the opportunity to communicate with other people with the condition.
Viral infections
The above advice refers to the bacterial infections in the lungs. It is important to remember that people with bronchiectasis are more likely to pick up viral infections when these are circulating. General advice to avoid picking up infections includes:
Make sure you are up to date with your vaccinations.
Wash your hands before meals and after being in contact with others
Do not visit anyone with a cold or a chest infection, and ask people not to visit you when they are unwell
Online resources and discussion forums
These online resources have been recommended by people with experience of bronchiectasis.
We do not endorse or moderate any of these resources or online groups so do think about the details you share and check any advice offered with a healthcare professional.
English
Finnish:
Italian:
Dutch:
Further information
Get involved in research
To find out more about how you can get involved in research, read about how ELF works with patients.
You can also search these databases for current bronchiectasis trials taking place across the world:
- EU Clinical Trials Register
- Clinicaltrials.gov (US National Library of Medicine) – covers 200 countries.
ERS guidelines on the management of bronchiectasis
These guidelines from ERS (European Respiratory Society) include the most appropriate investigation and treatment strategies for bronchiectasis and were produced by a group of experts on the topic, based on the best available published evidence.
Read a summary written for people with bronchiectasis to help you understand what was recommended in the original guideline.
Bronchiectasis events
This information was compiled as part of the bronchiectasis patient priorities project with the help of EMBARC and members of the ELF bronchiectasis patient advisory group.
EMBARC is a pan-European network committed to promoting clinical research and education in bronchiectasis, through sharing of protocols, research ideas and expertise.
If you want to access the latest data on bronchiectasis, visit the Lung Facts website
Launched by the International Respiratory Coalition and using data from the Global Burden of Disease study, Lung Facts provides the latest numbers on people living with lung disease by condition and by country.
Learn more





